How to Build Effective Risk Management in Healthcare: A Proven Patient Safety System
Some analyses suggest medical errors may be one of the leading causes of death in the U.S., but methodology and estimates vary widely. Healthcare risk management isn’t just important it saves lives.
The numbers paint a grim picture. Each year, about 400,000 patients in hospitals face some type of harm that could have been prevented. One out of every 20 patients experiences preventable harm during their medical care. The financial impact hits hard too adverse events cost our healthcare system $20 billion annually.
Clinical risk management strategies can substantially lower these numbers. Patient safety improves when healthcare teams tackle medication-related harm that affects one in 30 patients. Patient falls happen at rates of 3 to 5 per 1000 bed-days, but systematic approaches help prevent them. The stakes remain high 12% of preventable patient harm turns severe or results in death.
This piece offers proven frameworks that build patient safety systems that work. You’ll find ways to identify error mechanisms and create a culture where everyone owns safety. These strategies will protect your patients and organization, whether you’re handling healthcare associated infections or don’t deal very well with communication breakdowns.
Understanding the Types of Risks in Healthcare

Image Source: SlideEgg
Healthcare facilities deal with countless patient safety challenges every day. A good grasp of these risks helps create better risk management strategies.
Surgical, diagnostic, and medication errors
Surgical errors pose a major risk to patient safety. Surgical errors represent a significant share of adverse events, and a large fraction of malpractice claims against surgeons relate to surgical procedures.
Diagnostic errors impact millions of patients each year and remain the most common type of medical mistake. Doctor reviews show that harmful diagnostic errors affect at least 0.7% of adult patients. These errors lead to death or injury of 40,000 to 80,000 patients annually.
Medication errors stand as the most frequent and preventable cause of patient harm. These mistakes affect 1 in 30 patients, and more than a quarter of these cases turn severe or life-threatening. The prescribing or ordering stages account for nearly 50% of all medication errors.
Hospital-acquired infections and patient falls
Healthcare-associated infections show a global rate of 0.14% and grow by 0.06% yearly. Patients stay longer in hospitals because of these infections, which also increase antimicrobial resistance and cause preventable deaths. These infections affect up to 1 in 20 hospitalized patients.
Patient falls top the list of adverse events in hospitals. They occur 3 to 5 times per 1000 bed-days. One-third of these cases result in injury. An injurious fall costs about $35,365, while non-injurious falls cost around $36,776.
Communication breakdowns and equipment failures
Communication breakdowns cause most harmful medical errors. About 67% of these errors happen during patient handoffs between providers. The Joint Commission’s research reveals that poor communication during patient handovers causes 80% of serious medical errors.
Equipment failures create another critical risk area. Patient harm often results from faulty hospital equipment. Manufacturing defects, poor maintenance, or user error can cause these failures. Additional risks come from improper handling, wrong diagnoses, unsuitable treatments, or operator mistakes.
Identifying Root Causes of Medical Errors
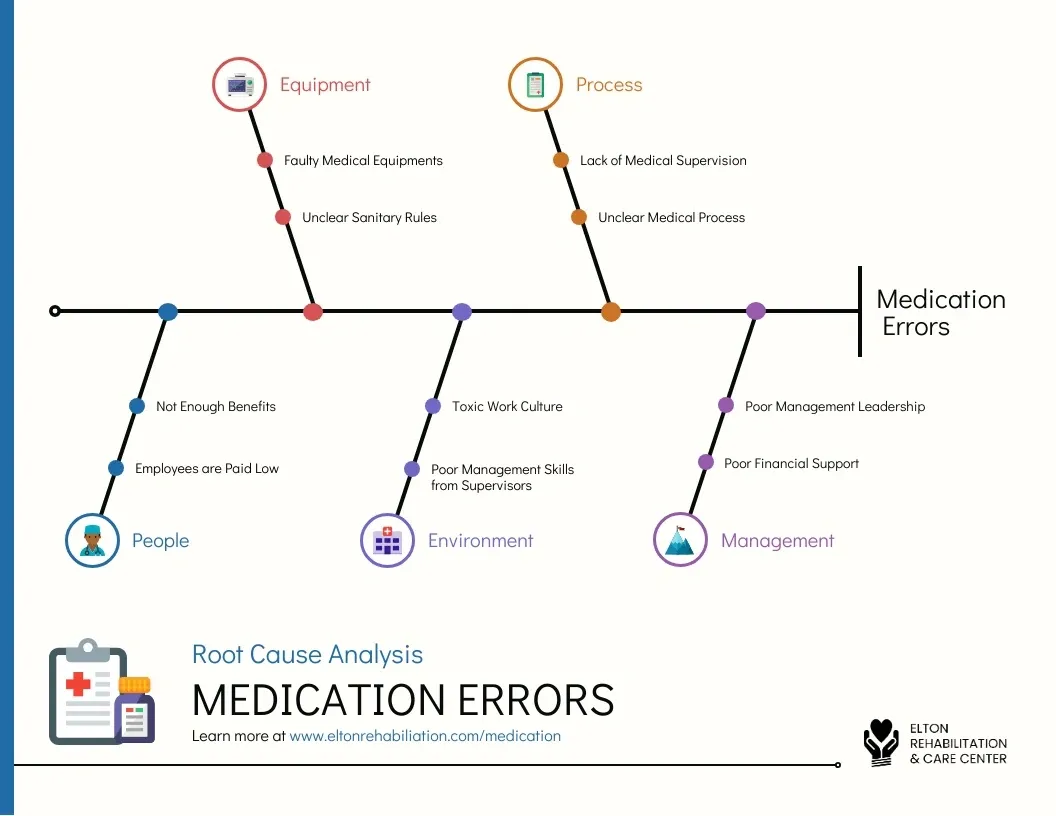
Image Source: Venngage
Medical errors have deeper roots than what we see on the surface. Healthcare risk management works best when we understand why adverse events happen in the first place.
Active vs. latent errors
Medical errors split into two main categories. Active errors happen at the “sharp end” of care when healthcare providers make immediate mistakes while treating patients. These mistakes include giving wrong medications, surgical errors, or incorrect diagnoses.
Latent errors tell a different story. They hide at the “blunt end” as system flaws that stay hidden until specific conditions bring them to light. These hidden problems can lurk for years before causing harm. Research shows almost every major failure stems from a system flaw that surfaces through an act someone did or didn’t do.
System design flaws and human factors
Human factors affect error rates by a lot. Sleep deprivation increases reaction time and makes it harder to notice alarms. Cognitive overload leads to poor decisions. Research shows long shifts, distractions, and pressure reduce care quality and make clinicians more likely to make mistakes.
System design problems include badly designed medical devices, uncoordinated care processes, and fragmented health systems. EHR-related error analysis revealed seven major safety issues. These range from data entry problems to poor alerts, weak system connections, and confusing screen displays.
The role of clinical risk management
Clinical risk management wants to find causes, not point fingers. This view recognizes that healthcare workers make mistakes because systems fail, not because they lack skills.
Root cause analysis (RCA) gives us a well-laid-out way to investigate serious adverse events. It helps us spot both active and latent errors systematically. Old methods blamed individuals, but modern RCA looks at organization factors, equipment problems, environment, staffing, and communication issues.
Risk management works best with adverse event reporting systems where staff can report critical incidents without fear. This helps spot patterns and fix systemic issues instead of just treating symptoms.
Building a Patient Safety System: Key Strategies
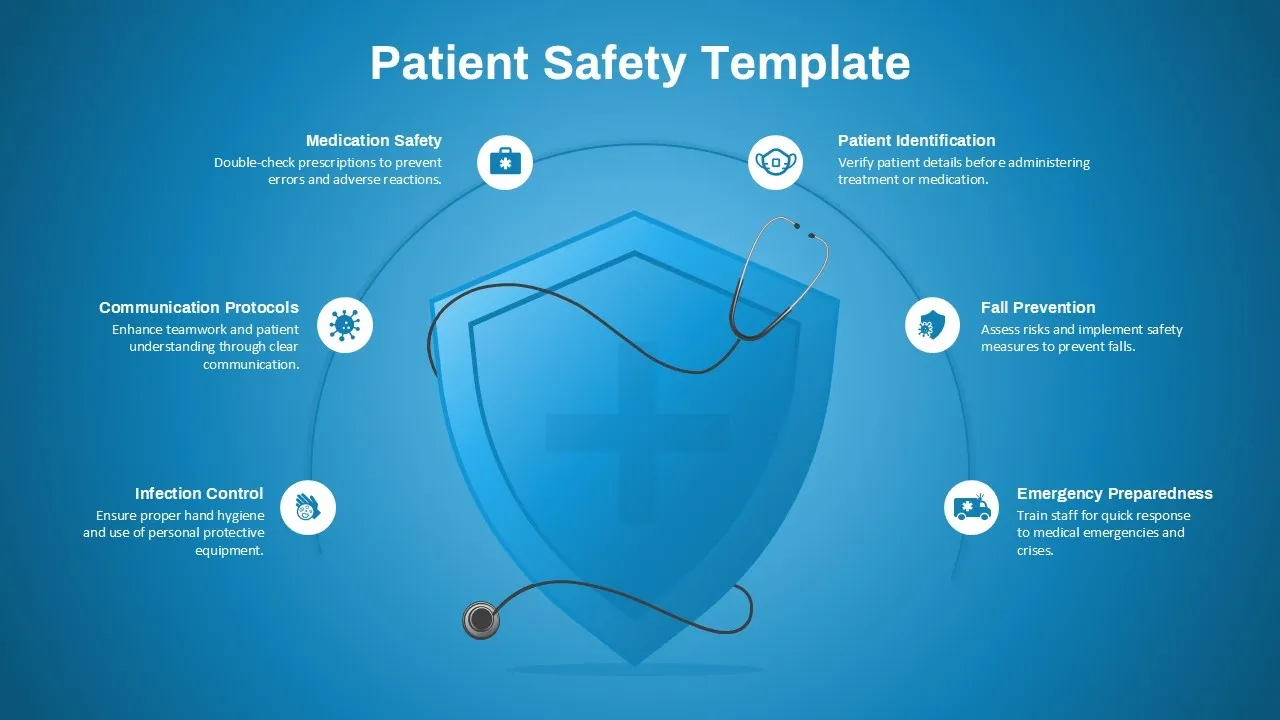
Image Source: SlideKit
Healthcare safety systems need multiple coordinated strategies to work well. Expert guidance on clinical protocols, safety indicators, and infection prevention best practices helps improve patient outcomes. These approaches are the foundations of successful risk management in healthcare.
Implementing checklists and safety protocols
Research shows surgical checklists reduce mortality by 47% [link_1] and complications by 36%. These well-laid-out tools create “time-outs” where providers focus only on patient safety concerns. A good checklist verifies patient identity, marks surgical sites, reconciles medications, and addresses predicted recovery concerns. EMR medication verification systems also reduce administration errors by confirming correct dosages and checking patient allergies.
Using patient safety indicators to track progress
Patient safety indicators (PSIs) offer measurable data on harm prevention effectiveness. These indicators include numerator and denominator specifications with risk-adjustment capabilities to track trends over time. The Agency for Healthcare Research and Quality developed PSIs to capture potentially preventable events in acute care settings. Specialty societies later created specific indicators for surgical, laboratory, and cardiac procedures.
Encouraging error reporting and transparency
Effective reporting systems need four essential elements:
- A supportive environment that protects reporter privacy
- Reports from a variety of personnel
- Quick sharing of event summaries
- Clear methods to develop action plans
Training staff on risk awareness and mitigation
Staff education builds risk awareness and enables healthcare workers to signal potential hazards early. Teams with proper training develop a risk-based mindset and feel more confident to speak up about safety concerns.
Creating a Culture of Safety and Accountability
A strong safety culture forms the foundation of effective risk management in healthcare. The safety environment serves as a base that supports all other safety initiatives.
Leadership commitment to safety
Hospital boards need to understand safety’s importance and take active part in safety initiatives to create a culture that prioritizes patient protection. Staff members have better perceptions of safety climate when hospital leaders provide useful feedback and stay available. Safety culture improves substantially when executives hold frank discussions with frontline workers about safety concerns through leadership walkrounds and address raised issues promptly.
Interprofessional collaboration and communication
Poor communication and collaboration cause about 70% of adverse events. Teams with high psychological safety share critical patient information more openly and report safety events more often while actively participating in teamwork. Clear information exchange becomes easier with communication frameworks like SBAR (Situation-Background-Assessment-Recommendation).
Empowering staff to speak up
Staff members need supportive environments that give them the ability to voice safety concerns. Research shows that employee’s perceptions of psychological safety improve when they rate their leaders highly. Staff members identify potential hazards more readily when organizations establish non-punitive reporting systems.
Monitoring and feedback loops for continuous improvement
Quality improvement requires constant evaluation of current performance and potential areas of enhancement. Clinicians make better diagnostic decisions through patient outcome feedback. Leaders should collect data, guide discussions, spot trends that need system-wide improvements, and ensure proper handling of errors.
Conclusion
Risk management serves as a vital lifeline in healthcare where patient safety is at stake. This piece shows how methodical approaches can reduce preventable harm that affects thousands of patients each year.
Identifying risks is the first significant step to create safer healthcare. Understanding threats like surgical errors, medication mistakes, hospital-acquired infections, and communication failures helps develop targeted prevention strategies.
Finding why it happens instead of just fixing symptoms will improve the system genuinely. Most errors come from system failures, not individual mistakes. This changes the focus from blame to practical solutions.
Patient safety systems work best with proven frameworks. Checklists, safety protocols, and tracking indicators add structure to risk management work. Error reporting systems let teams learn from mistakes. Staff training turns safety from theory into everyday practice.
Safety culture forms the foundation of all risk management plans. Leadership’s dedication, teamwork between professionals, and staff empowerment create spaces where everyone owns safety. Regular monitoring helps organizations adapt to new threats.
Safer healthcare needs dedication, watchfulness, and organized methods. These strategies protect patients and healthcare organizations from avoidable harm. Patient safety isn’t just about following rules or saving money – it’s a basic ethical duty at healthcare’s core.